3/15/2025 UPDATE – For the time being, the ALARM ACT initiative has been merged with HB 788, which was filed by Representative Kim Moser in the Kentucky General Assembly. For more information check out the KYSAM advocacy HB 788 website: https://www.kysam.org/news
Kentucky House Bill 788 supports increased access to buprenorphine by empowering Kentucky’s providers to treat patients with evidence-based care. Check out this 9 minute video of Dr. Murphy’s recent testimony in Kentucky’s capital city: https://www.youtube.com/watch?v=3lILI0x4TXo
The salient issues remain consistent with the ALARM ACT initiative, thus I’m keeping this post on the website to provide historical context supporting our efforts to save lives.
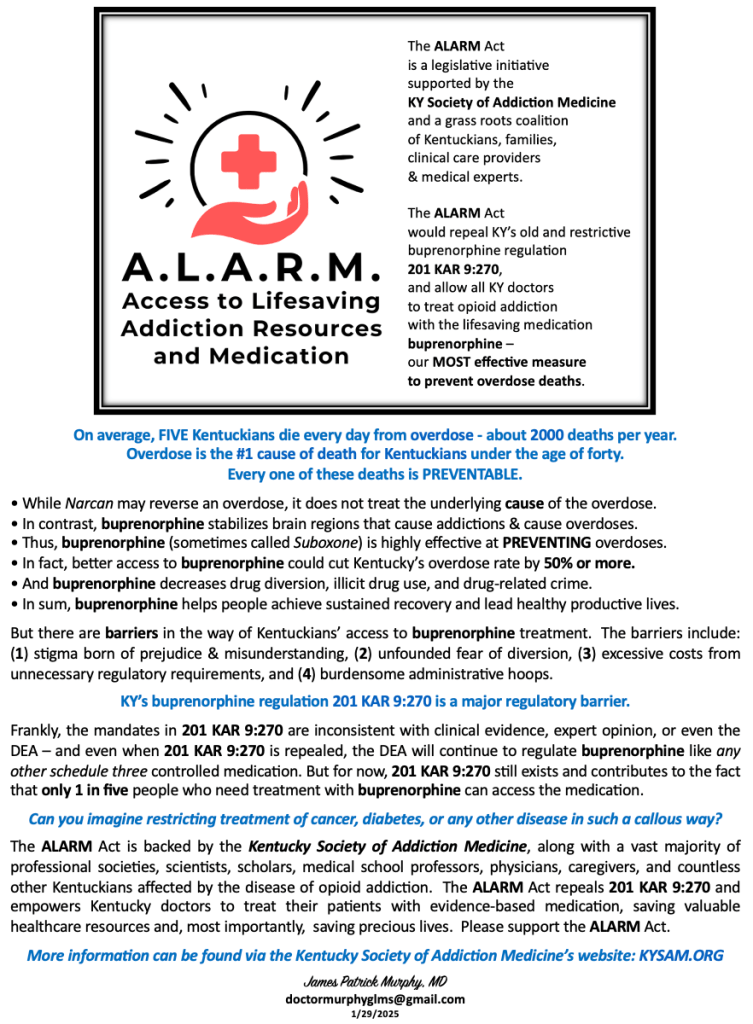
ALARM Act one-page advocacy brief
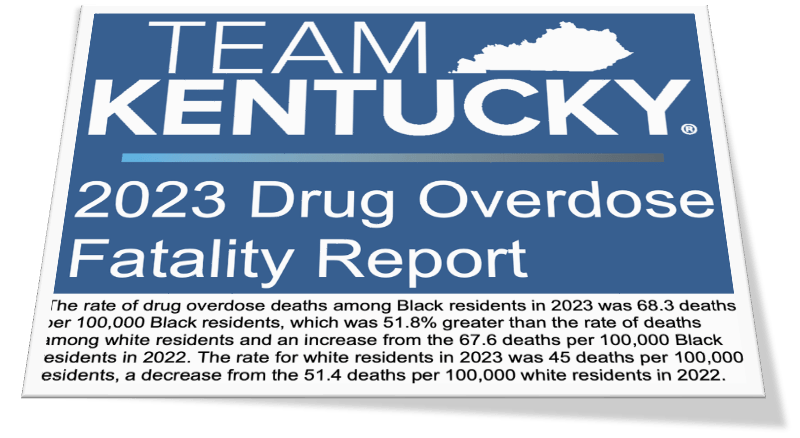
On average, FIVE Kentuckians die every day from overdose – about 2000 deaths per year.
Overdose is the #1 cause of death for Kentuckians under the age of forty.
Every one of these deaths is PREVENTABLE.
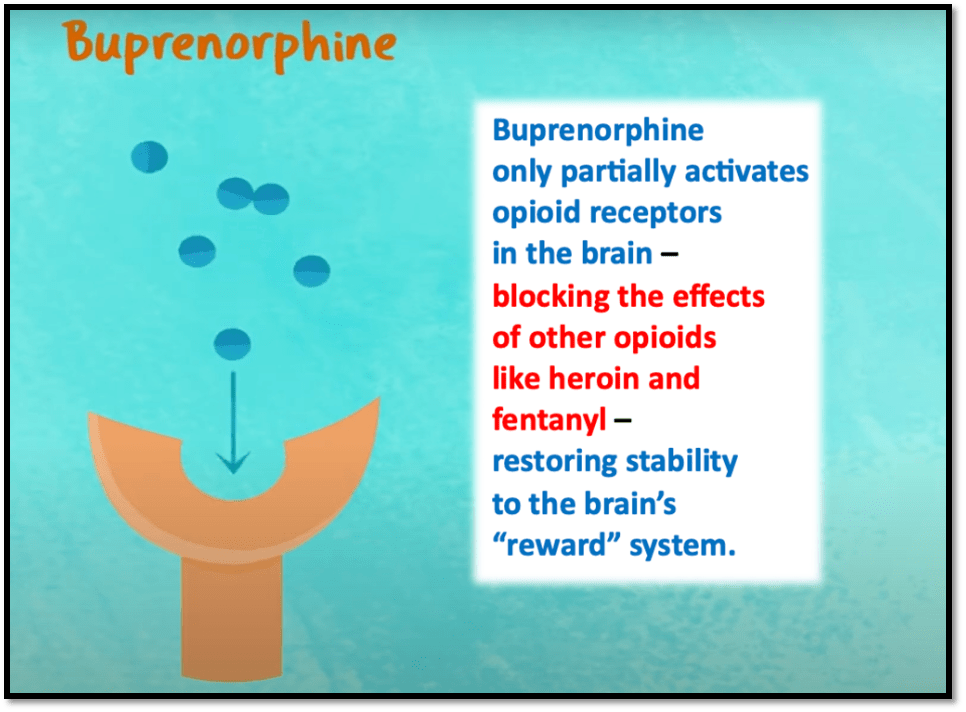
• While Narcan may reverse an overdose, it does not treat the underlying cause of the overdose.
• In contrast, buprenorphine stabilizes brain regions that cause addictions & cause overdoses.
• Thus, buprenorphine (sometimes called Suboxone) is highly effective at PREVENTING overdoses.
• In fact, better access to buprenorphine could cut Kentucky’s overdose rate by 50% or more.
• And buprenorphine decreases drug diversion, illicit drug use, and drug-related crime.
• In sum, buprenorphine helps people achieve sustained recovery and lead healthy productive lives.
But there are barriers in the way of Kentuckians’ access to buprenorphine treatment. The barriers include: (1) stigma born of prejudice & misunderstanding, (2) unfounded fear of diversion, (3) excessive costs from unnecessary regulatory requirements, and (4) burdensome administrative hoops.
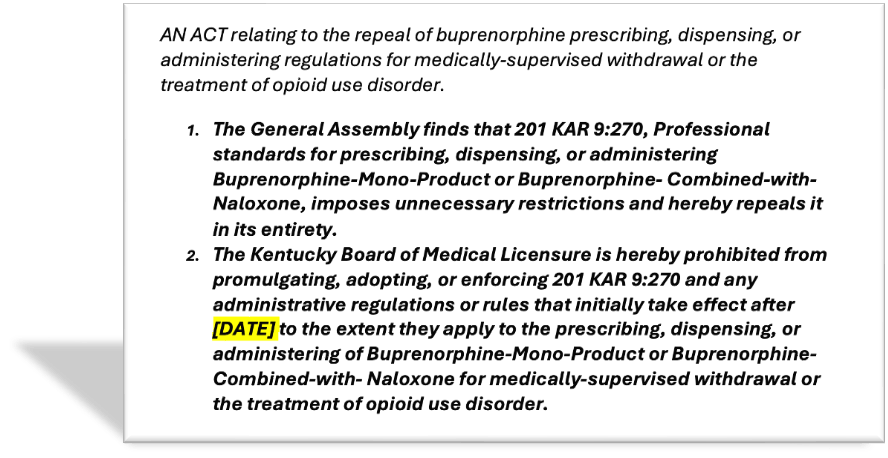
KY’s buprenorphine regulation 201 KAR 9:270 is a major regulatory barrier.
Frankly, the mandates in 201 KAR 9:270 are inconsistent with clinical evidence, expert opinion, or even the DEA – and even when 201 KAR 9:270 is repealed, the DEA will continue to regulate buprenorphine like any other schedule three controlled medication. But for now, 201 KAR 9:270 still exists and contributes to the fact that only 1 in five people who need treatment with buprenorphine can access the medication.
Can you imagine restricting treatment of cancer, diabetes, or any other disease in such a callous way?
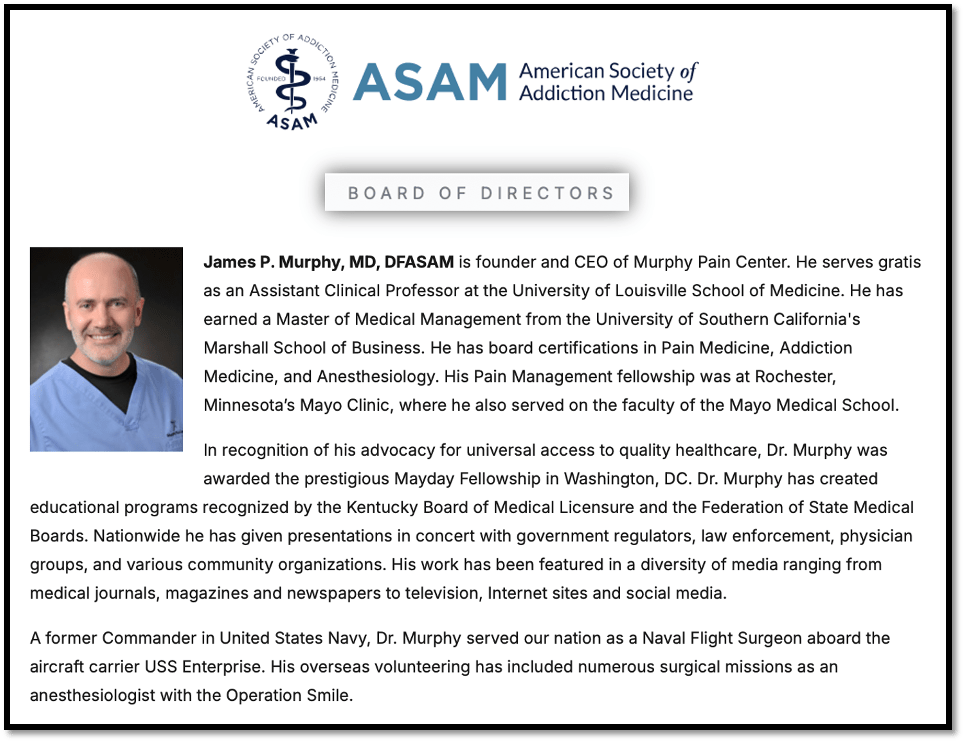
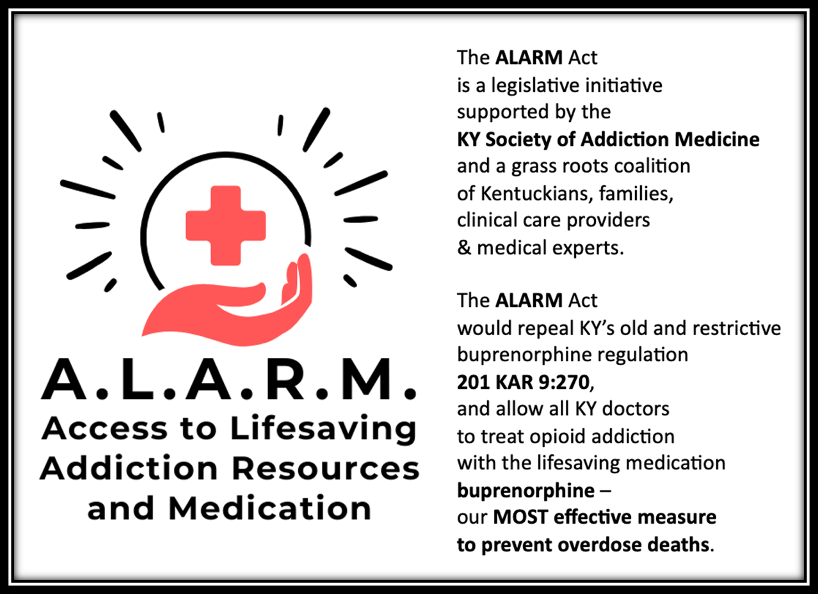
The ALARM Act is backed by the Kentucky Society of Addiction Medicine, along with a vast majority of professional societies, scientists, scholars, medical school professors, physicians, caregivers, and countless other Kentuckians affected by the disease of opioid addiction. The ALARM Act repeals 201 KAR 9:270 and empowers Kentucky doctors to treat their patients with evidence-based medication, saving valuable healthcare resources and, most importantly, saving precious lives. Please support the ALARM Act.
More information can be found via the Kentucky Society of Addiction Medicine’s website: KYSAM.ORG
doctormurphyglms@gmail.com
1/29/2025