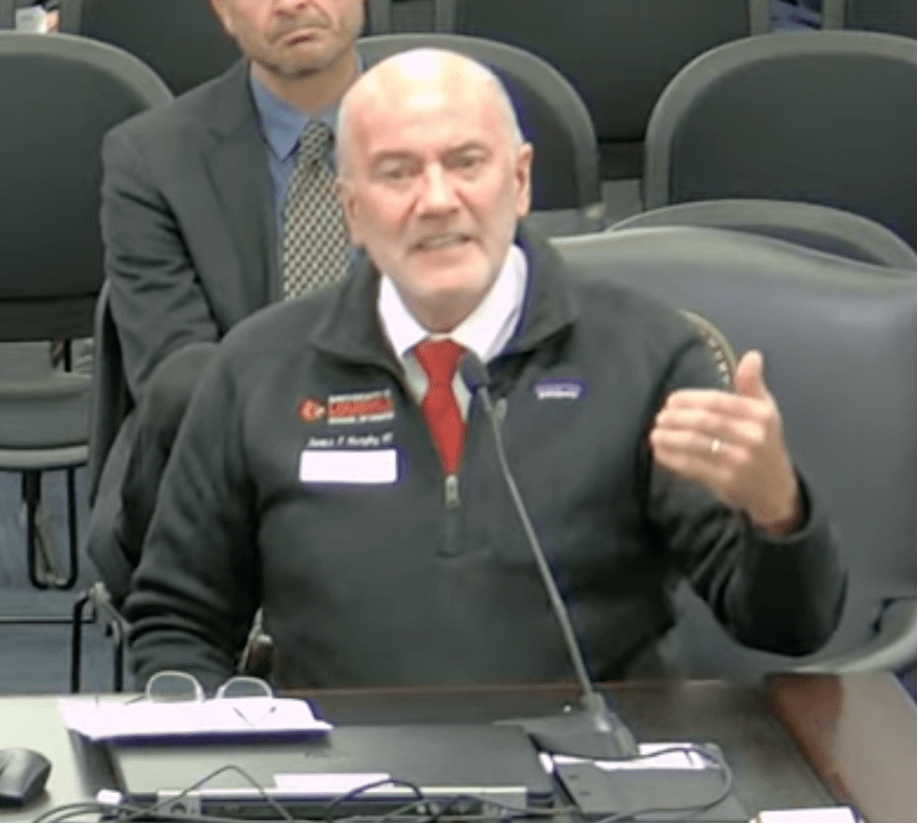
Note: The letter is still open for signatures. Email James Patrick Murphy MD at jpmurphy.mpc@gmail.com to join the support for HB 153 / SB 82.
Current as of March 7, 2026
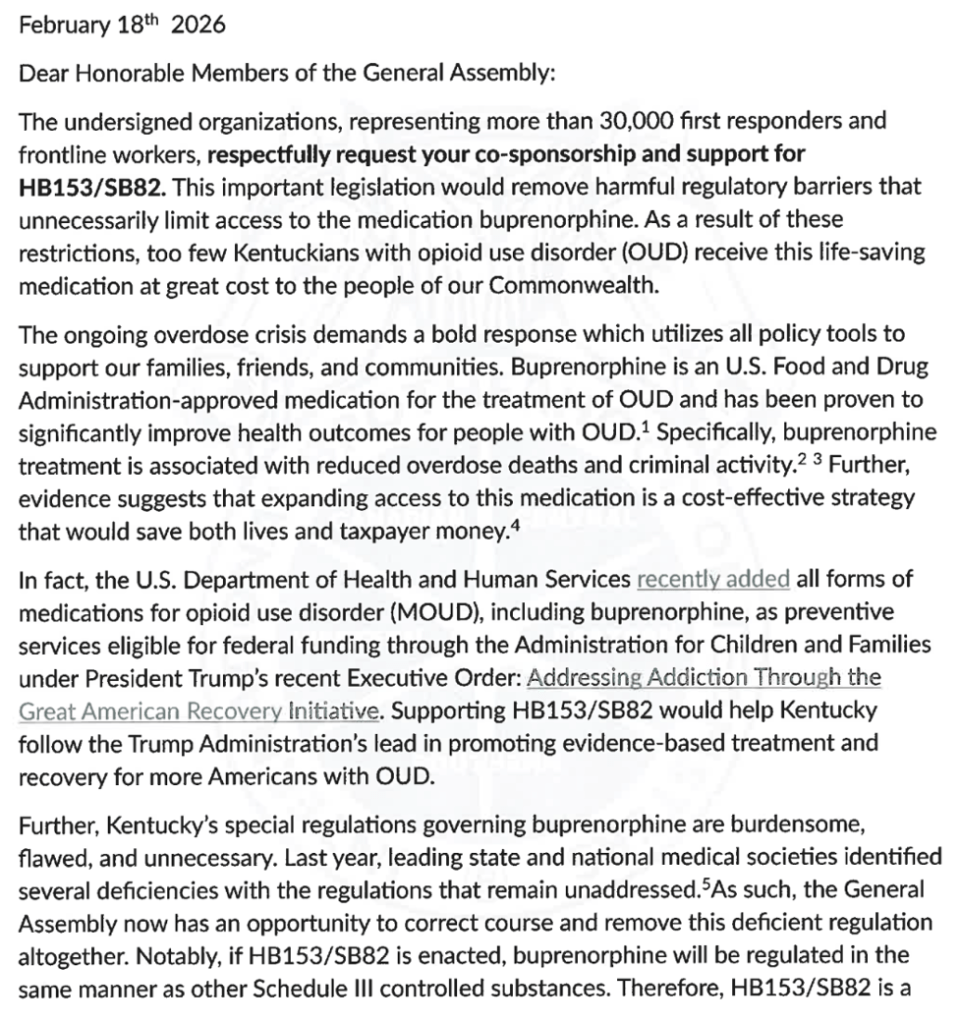
Dear Honorable Members of the General Assembly:
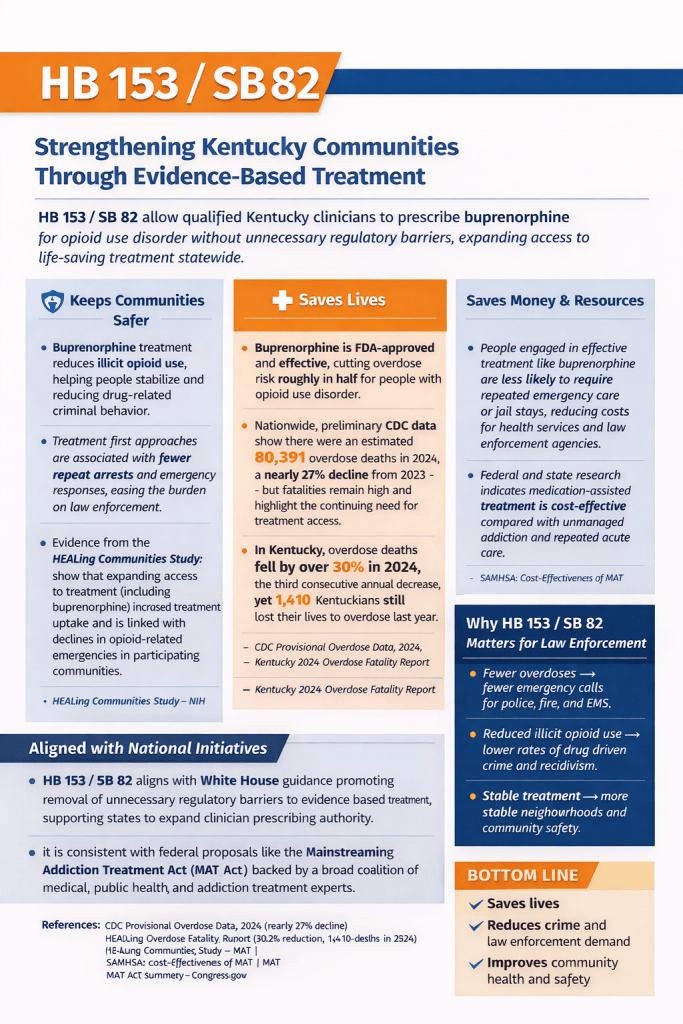
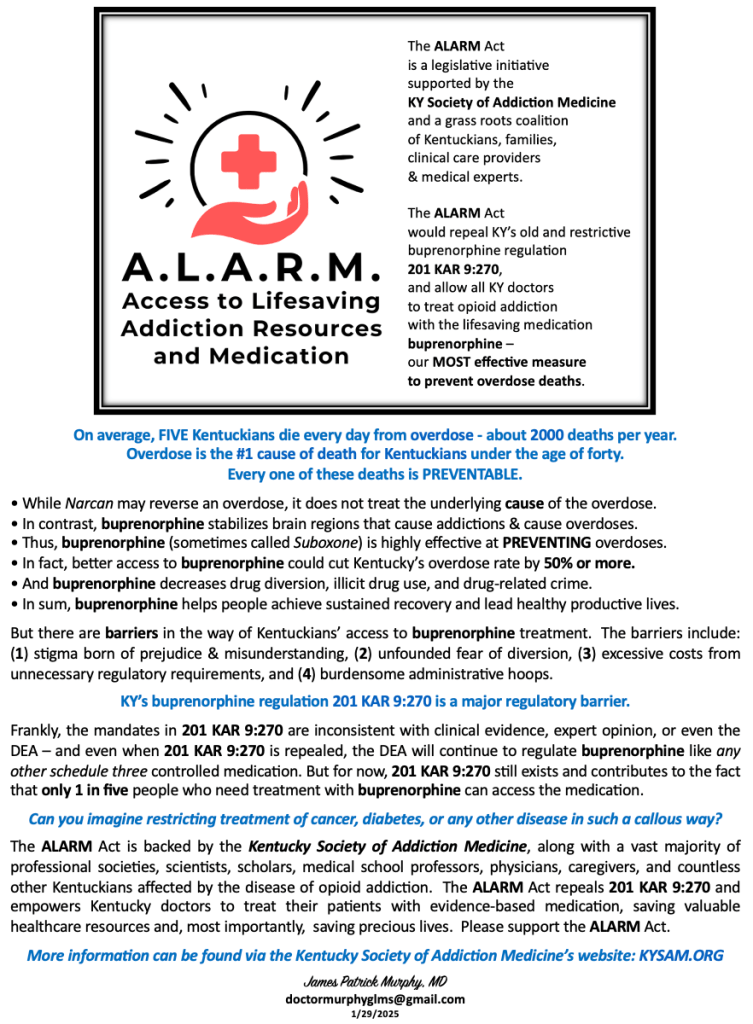
The undersigned organizations, representing more than twenty-four law enforcement, medical societies and patient advocacy groups, respectfully request your co-sponsorship and support for HB153 / SB82. This important legislation would remove harmful regulatory barriers that unnecessarily limit access to the medication buprenorphine. As a result of these restrictions, too few Kentuckians with opioid use disorder (OUD) receive this life-saving medication at great cost to the people of our Commonwealth.
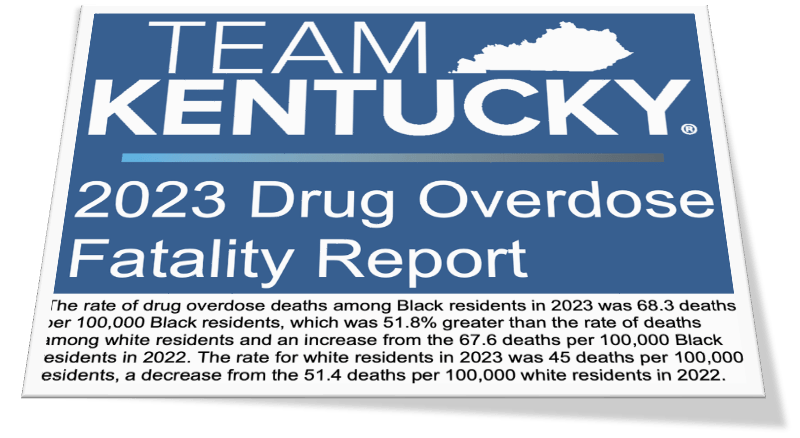
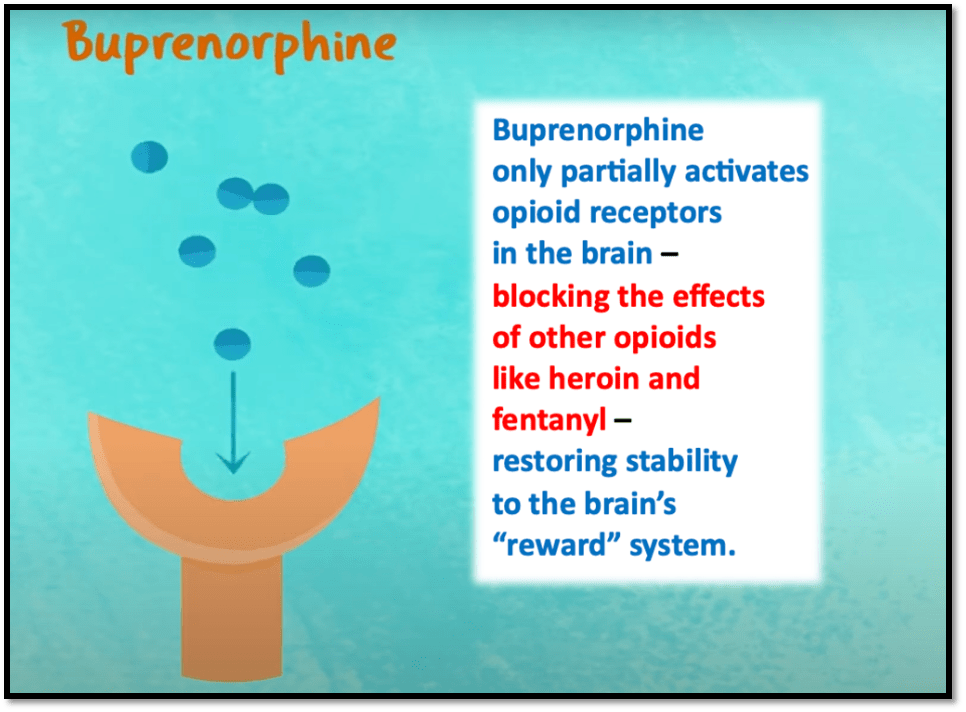
The ongoing overdose crisis demands a bold response which utilizes all policy tools to support our families, friends, and communities. Buprenorphine is an U.S. Food and Drug Administration-approved medication for the treatment of OUD and has been proven to significantly improve health outcomes for people with OUD.[i] Specifically, buprenorphine treatment is associated with reduced overdose deaths and criminal activity.[ii] [iii] Further, evidence suggests that expanding access to this medication is a cost-effective strategy that would save both lives and taxpayer money.[iv]
In fact, the U.S. Department of Health and Human Services recently added all forms of medications for opioid use disorder (MOUD), including buprenorphine, as preventive services eligible for federal funding through the Administration for Children and Families under President Trump’s recent Executive Order: Addressing Addiction Through the Great American Recovery Initiative. Supporting HB153 / SB82 would help Kentucky follow the Trump Administration’s lead in promoting evidence-based treatment and recovery for more Americans with OUD.
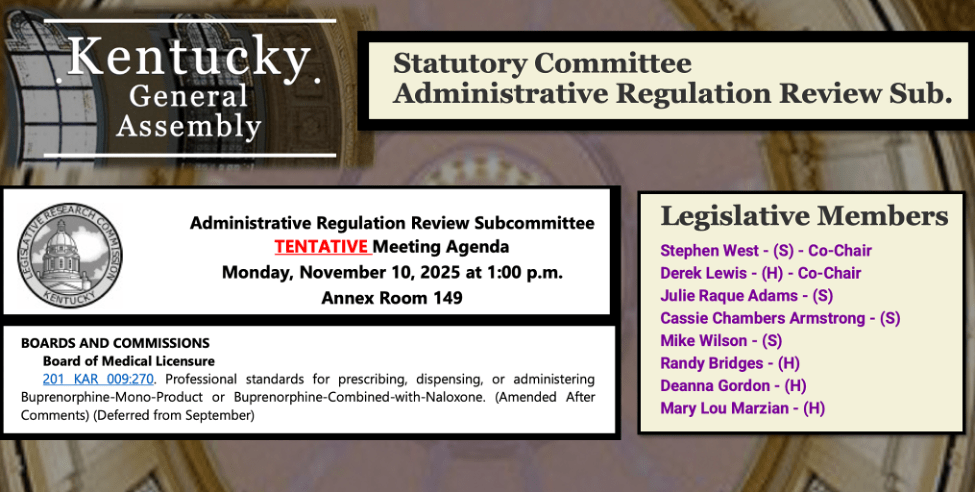
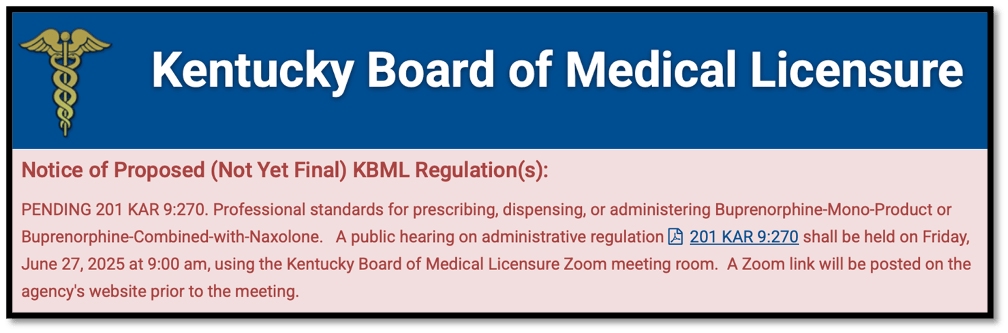
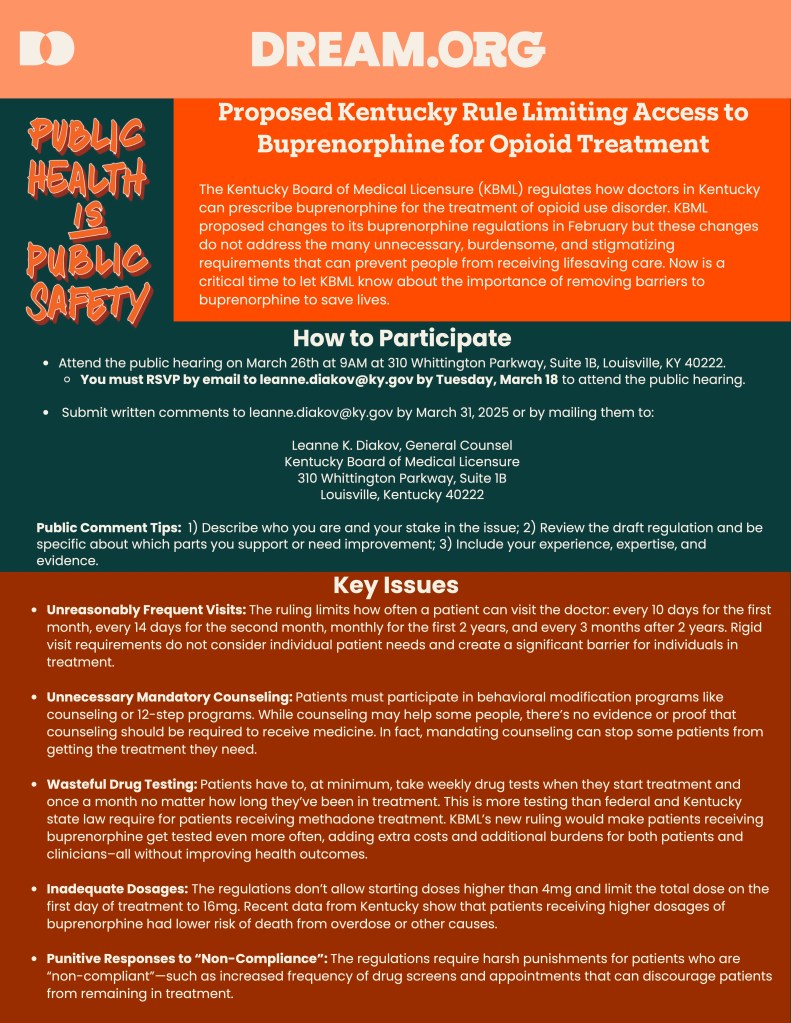
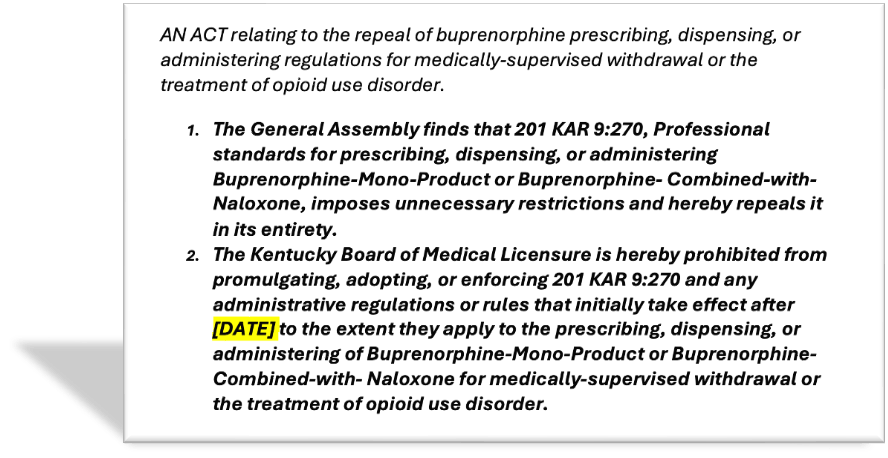
Further, Kentucky’s special regulations governing buprenorphine are burdensome, flawed, and unnecessary. Last year, leading state and national medical societies identified several deficiencies with the regulations that remain unaddressed.[v]As such, the General Assembly now has an opportunity to correct course and remove this deficient regulation altogether. Notably, if HB153 / SB82 is enacted, buprenorphine will be regulated in the same manner as other Schedule III controlled substances. Therefore, HB153 / SB82 is a common-sense effort to simplify our regulatory scheme and return treatment decisions to clinicians and patients.
Opponents of this legislation warn that removing special regulations on buprenorphine would increase the risk that this medication is diverted. However, evidence suggests that most people use any diverted buprenorphine to self-treat withdrawal and more strictly regulating buprenorphine may actually increase diversion risk.[vi]As such, we must work to ensure that evidence-based treatment for OUD is more accessible in Kentucky. Enacting HB153 / SB82 is a significant step towards accomplishing that goal.
Ultimately, HB153 / SB82 is sensible legislation that would reverse flawed regulations and promote treatment, remission, and recovery for more Kentuckians. As such, we are proud to support this legislation and respectfully urge your co-sponsorship and support for its passage soon. Thank you for your consideration.
Sincerely,
Signatories in Support of HB 153 / SB 82 (Updated March 7, 2026):
Kentucky Society of Addiction Medicine
Kentucky Sheriffs’ Association
Kentucky Association of Fire Chiefs
Kentucky Association of Criminal Defense Lawyers
Kentucky Psychiatric Medical Association
American Academy of Addiction Psychiatry
Kentucky Psychological Association
Kentucky Mental Health Coalition
Kentucky Academy of Physician Assistants
Kentucky Pharmacists Association
Kentucky Society of Health-System Pharmacists
Kentucky Ambulance Providers Association
Division of Palliative Medicine, University of Louisville School of Medicine
Cardinal Street Medicine — UofL School of Medicine Students
Doctors for America — Kentucky Membership
Kentucky Social Work Advocacy, Justice, and Leadership
Police, Treatment, and Community Collaborative
Americans for Prosperity – Kentucky
Kentucky Center for Economic Policy
Law Enforcement Action Partnership
Additionally:
Appalachian Regional Healthcare officially supports HB 153 / SB 82 – ARH, with more than 1,300 providers across its multi-state system, is the largest provider of care and the single largest employer in southeastern Kentucky.
Leadership representing over 30,000 first responders and frontline workers—including Louisville EMS and MetroSafe— support HB 153 / SB 82.
Kentucky Professional Fire Fighters, representing forty-three fire fighter and EMS unions throughout Kentucky, officially supports HB 153 / SB 82.
Kentucky Firefighter’s Association, serving and promoting the interests of all firefighters in the Commonwealth of Kentucky, officially supports HB 153/ SB 82.
Kentucky Voices for Health has joined the coalition supporting HB 153 / SB 82.
The Greater Louisville Medical Society independently expressed strong support for HB 153 / SB 82 (full letter to the General Assembly attached below), stating:
HB 153 / SB 82 is sensible legislation that would update flawed regulations and promote treatment, remission, and recovery for more Kentuckians. We are proud to support this legislation and respectfully urge your co-sponsorship and support for its passage soon.
Consistent with the goals of HB 153 / SB 82, the following organizations have previously called for the revision or repeal of Kentucky’s buprenorphine regulation, 201 KAR 9:270:
Kentucky Medical Association 2025 House of Delegates
American Academy of Family Physicians
Kentucky Academy of Family Physicians
American Society of Addiction Medicine
American Psychiatric Association
American Academy of Addiction Psychiatry
American College of Obstetricians and Gynecologists (ACOG)
Kentucky Section of the American College of Obstetricians and Gynecologists
Association for Multidisciplinary Education and Research in Substance Use and Addiction
[i] U.S. Department of Health and Human Services. (2026, February 2). ACF Expands Access to Medications for Opioid Use Disorder for At-Risk Families. Administration for Children & Families. https://acf.gov/media/press/2026/acf-expands-access-medications-opioid-use-disorder-risk-families
[ii] Santo, T., Clark, B., Hickman, M., Grebely, J., Campbell, G., Sordo, L., Chen, A., Tran, L. T., Bharat, C., Padmanathan, P., Cousins, G., Dupouy, J., Kelty, E., Muga, R., Nosyk, B., Min, J., Pavarin, R., Farrell, M., & Degenhardt, L. (2021). Association Between Length of Buprenorphine or Methadone Use and Nonprescribed Opioid Use Among Individuals with Opioid Use Disorder: A Cohort Study. JAMA Psychiatry, 78(9), 979. https://doi.org/10.1001/jamapsychiatry.2021.0976
[iii] Molero, Y., Zetterqvist, J., Binswanger, I. A., Hellner, C., Larsson, H., & Fazel, S. (2018). Medications for Alcohol and Opioid Use Disorders and Risk of Suicidal Behavior, Accidental Overdoses, and Crime. American Journal of Psychiatry, 175(10), 970–978. https://doi.org/10.1176/appi.ajp.2018.17101112
[iv] Fairley, M., Humphreys, K., Joyce, V. R., Bounthavong, M., Trafton, J., Combs, A., Oliva, E. M., Goldhaber-Fiebert, J. D., Asch, S. M., Brandeau, M. L., & Owens, D. K. (2021). Cost-effectiveness of Treatments for Opioid Use Disorder. JAMA Psychiatry, 78(7), 767. https://doi.org/10.1001/jamapsychiatry.2021.0247
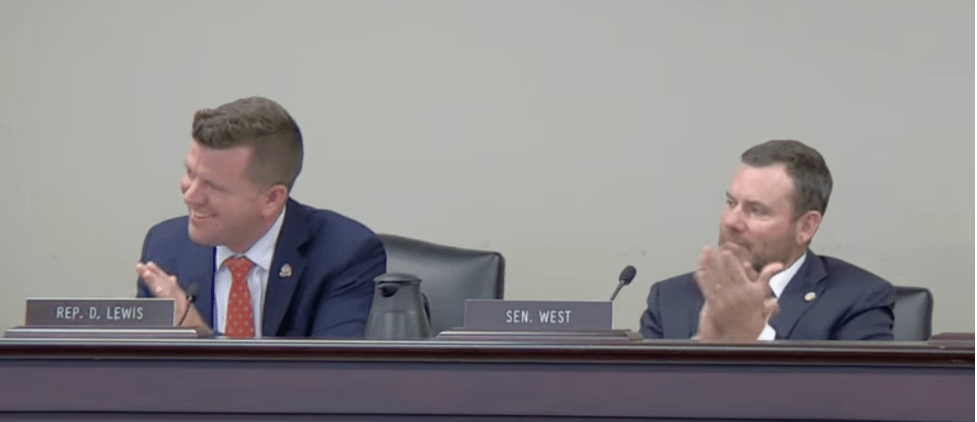
[v] October 2025 Letter: https://apps.legislature.ky.gov/CommitteeDocuments/3/42171/ASAM-KSAM%20Statement%20re%20201%20KAR%209-270%20%28October%202025%29.pdf
[vi] Rubel, S. K., Eisenstat, M., Wolff, J., Calevski, M., & Mital, S. (2023). Scope of, Motivations for, and Outcomes Associated with Buprenorphine Diversion in the United States: A Scoping Review. Substance Use & Misuse, 58(5), 685–697. https://doi.org/10.1080/10826084.2023.2177972