HERE’S THE LATEST: The Kentucky Board of Medical Licensure (KBML) filed their updated version of 201 KAR 9:270 (the buprenorphine regulation) and scheduled an in-person public hearing for March 26, 2025. However, KBML cancelled this hearing due to an overwhelming number of requests by speakers to be heard. KBML has now rescheduled the hearing for June 27, 2025, only this time it’s not in-person. It’s a Zoom meeting! They have not posted the link yet, so stay tuned and monitor the KBML website, link: https://kbml.ky.gov/Pages/index.aspx
Please mark your calendar for June 27th and spread the news. To review, below is a call to action from Dream.org sent prior to the cancelled March 26th hearing – NOW JUNE 27. The same issues are still at stake. Your voice is needed now more than ever! Even if you only Zoom in for thirty seconds. YOUR WRITTEN COMMENTS MATTER TOO! THANK YOU!

Dear Friends, Neighbors, and Colleagues,
Now is the time to take action! Your voice can make a difference in Kentucky. A simple email could help save lives. Here’s how: Send an email to the Kentucky Board of Medical Licensure (KBML) via
Leanne K. Diakov, KBML General Counsel at leanne.diakov@ky.gov
To make it easier, simply click on this LINK, where you’ll find a helpful brief to guide you in crafting and sending your email to leanne.diakov@ky.gov
NOTE: KBML HAS RESCHEDULED THE PUBLIC HEARING FOR JUNE 27, 2025, AND ARE ACCEPTING EMIALS AND WRITTEN COMMENTS THROUGH JUNE 27.
https://mailchi.mp/kypar/take-1-minute-to-make-a-differencesave-lives?e=411f28ea2
Tell KMBL that you do not support the proposed changes Kentucky’s buprenorphine regulation, and you believe Kentucky would be better served by eliminating the entire regulation known as 201 KAR 9:270.
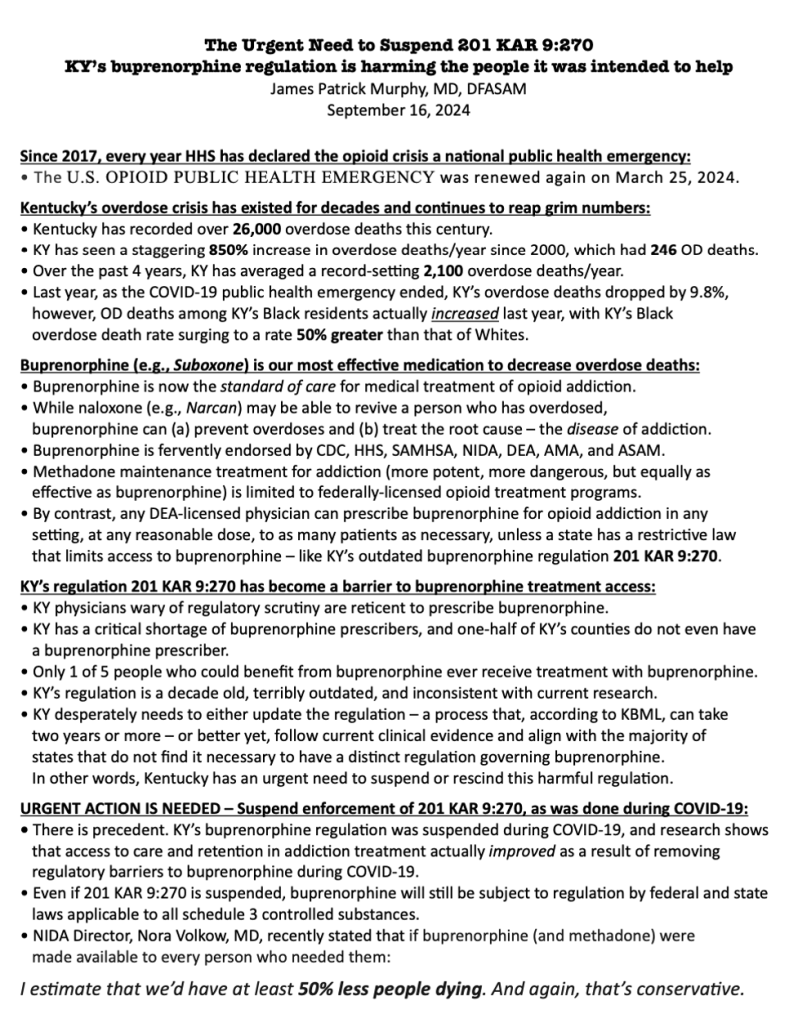
The Kentucky Board of Medical Licensure (KBML) is nearing the final stages of updating the regulation 201 KAR 9:270, which governs the treatment of Opioid Use Disorder with buprenorphine in Kentucky. Even with the proposed changes, this regulation remains flawed and harmful, and KBML has yet to fully acknowledge the impact. You don’t have to take my word for it. Read it for yourself at https://apps.legislature.ky.gov/law/kar/titles/201/009/270/REG/
Unfortunately, KBML’s proposed amendments do not address the damaging, stigmatizing policies first introduced in 2015. But you still have time to help alter this course. Until JUNE 27, you can make your voice heard with an email to KBML.
Despite input from hundreds of specialists, caregivers, and concerned Kentuckians calling for significant revisions to this harmful regulation, KBML has moved forward with publishing insufficient amendments to their outdated regulations on buprenorphine prescribing. Sadly, these amendments do little to improve the situation and further create barriers for patients seeking this life-saving treatment.
Kentucky is out of sync with the rest of the country. While federal guidelines have simplified and streamlined buprenorphine prescribing in recent years, Kentucky remains one of the few states enforcing stricter, punitive measures. Kentucky’s buprenorphine regulation (and its proposed amendments) are not only unsupported by evidence but also contribute to an increase in overdose deaths by limiting access to care.
If 201 KAR 9:270 and its proposed amendments are allowed to proceed, Kentucky will miss the opportunity to align itself with the latest scientific evidence, expert recommendations, and current federal guidelines. Continuing with Kentucky’s flawed regulation will only result in more preventable overdose deaths in our state.
If you’d like to read the experts’ perspectives, check out this letter from the Kentucky Society of Addiction Medicine to Governor Beshear: KYSAM Advocacy Letter link: https://www.kysam.org/kysam-advocacy
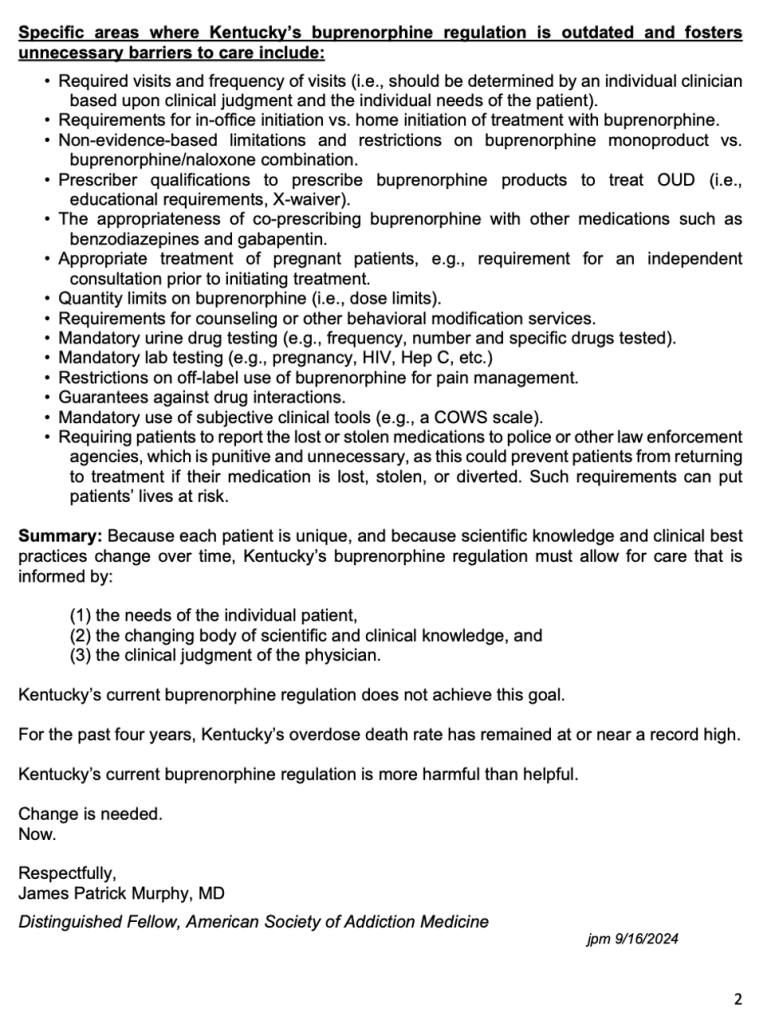
The proposed KBML regulation update includes several provisions that are not evidence-based, such as:
- Arbitrary dosage limits
- Mandatory behavioral and psychosocial interventions
- Inconsistent, compulsory appointment scheduling
- Non-evidence-based laboratory testing requirements
- Forced specialist referrals for certain patients
- A ban on using buprenorphine-naloxone for chronic pain
It’s time to take action!
Now through JUNE 27, you have the opportunity to speak up on behalf of those struggling with opioid use disorder. Email your comments to:
Leanne K. Diakov, KBML General Counsel: leanne.diakov@ky.gov
At the end of this post, you’ll find a sample letter that you can modify to share your personal perspective, if you wish. Personalizing your message can make a big impact!
Here’s why you should take action now:
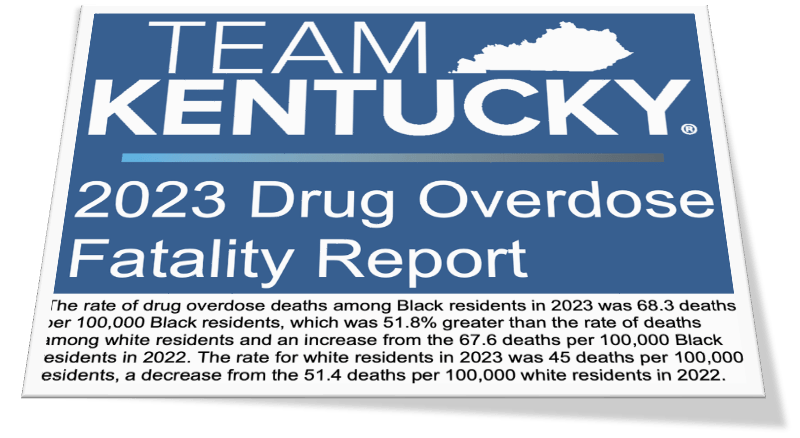
- Overdose is the leading cause of death for Kentuckians under 40.
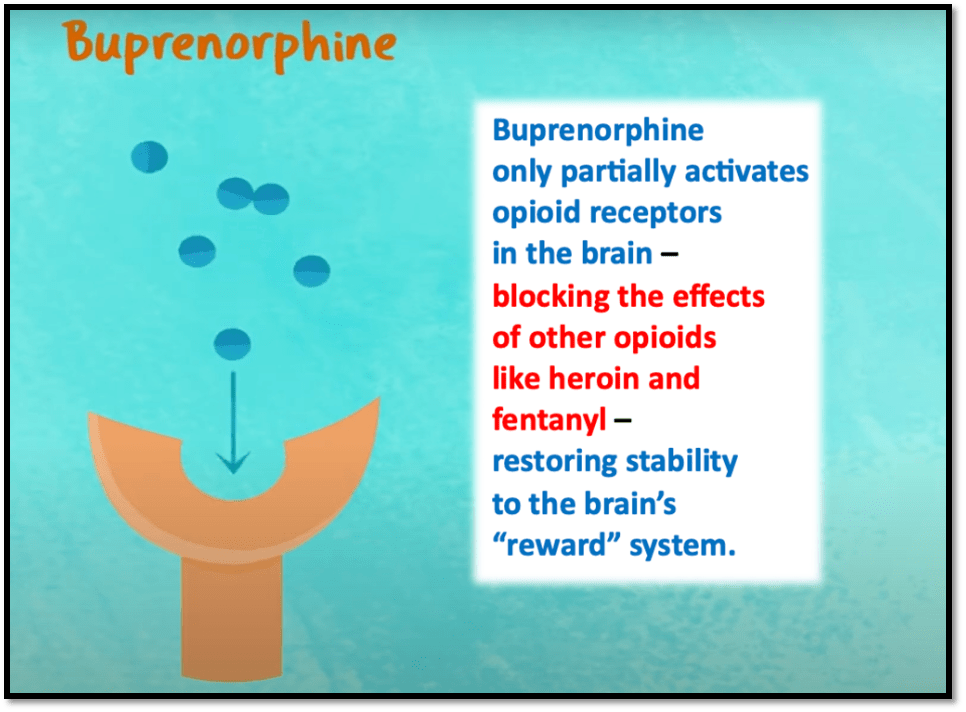
- The Director of the National Institute on Drug Abuse stated that if everyone who needs buprenorphine could access it, overdose deaths could be reduced by half.
- 201 KAR 9:270 is a barrier preventing Kentuckians from accessing this life-saving medication.
- And despite a tsunami of evidence proving the lifesaving effects of this medication, buprenorphine prescribing in Kentucky actually decreased last year! We must do better!
What more motivation do you need? Together, we can make a difference. Let your voice be heard!
Thank you for your support!
Sincerely,
James Patrick Murphy, MD, DFASAM
Dr. Murphy is Kentucky’s Regional Director for the American Society of Addiction Medicine and is a founding member of the American Medical Association’s Substance Use and Pain Care Task Force. He serves as an Assistant Clinical Professor for the University of Louisville School of Medicine and is board-certified in Anesthesiology, Pain Management, and Addiction Medicine.
***SAMPLE TEXT***
To:
Kentucky Board of Medical Licensure
Attention: Leanne K. Diakov, General Counsel
Email: leanne.diakov@ky.gov
RE: Public Comments on Proposed Amendments to 201 KAR 9:270
Dear Members of the Kentucky Board of Medical Licensure,
I am submitting my public comments on the proposed amendments to 201 KAR 9:270. Rather than addressing Kentucky’s overdose crisis, I am concerned that these proposed changes will only worsen the situation, creating additional barriers to care and limiting access to critical, lifesaving treatments. I respectfully urge the Board to prioritize evidence-based addiction treatment by rejecting these amendments and fully repealing this outdated and harmful regulation.
Expanding access to medications for opioid use disorder, such as buprenorphine, is crucial for reducing overdose deaths. Unfortunately, the proposed amendments directly contradict the guidance from several leading authorities, including the U.S. Department of Health and Human Services, the Drug Enforcement Administration, the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the Federation of State Medical Boards, all of which support broader access to buprenorphine-based treatments. The restrictions outlined in 201 KAR 9:270 would be counterproductive and could exacerbate health disparities, especially within marginalized communities.
If these proposed amendments are enacted, 201 KAR 9:270 will continue to contribute to Kentucky’s tragically high overdose death rate. I fully support the concerns raised by the Kentucky Society of Addiction Medicine, which has reviewed the proposed changes and deemed them insufficient. In light of these concerns, I strongly advocate for the full repeal of 201 KAR 9:270.
Thank you for considering the potential impact of these amendments on the health and well-being of Kentuckians. I urge the Board to prioritize evidence-based addiction treatment by rejecting these amendments and fully repealing this outdated and harmful regulation.
Sincerely,
[Your Name]
[Your Credentials/Professional Title, if applicable]
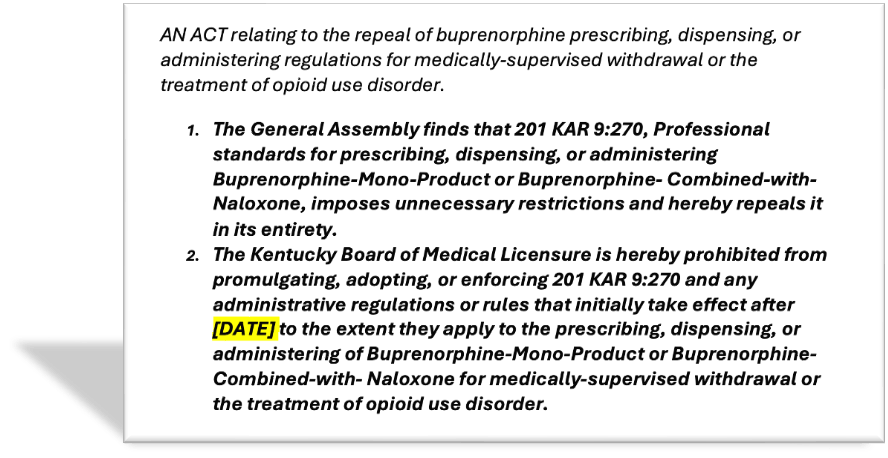
Kentucky House Bill 788 (currently in committee) supports increased access to buprenorphine by empowering Kentucky’s providers to treat patients with evidence-based care. Check out this 9 minute video of Dr. Murphy’s recent testimony in Kentucky’s capital city: https://www.youtube.com/watch?v=3lILI0x4TXo
More and more people and organizations are joining this cause…

















 https://jamespmurphymd.com/2014/03/18/is-there-method-to-this-march-madness
https://jamespmurphymd.com/2014/03/18/is-there-method-to-this-march-madness