On September 19, 2024, I did two things via the Kentucky Governor’s official website: (1) I requested a meeting, and (2) I sent him an email via https://governor.ky.gov/contact.
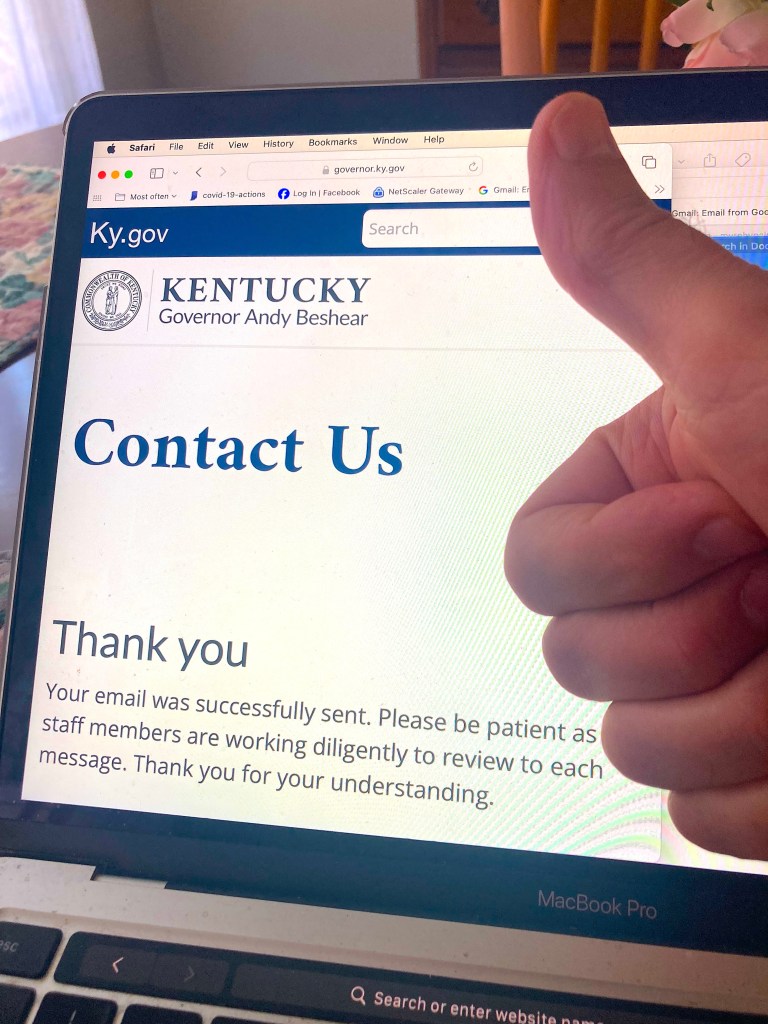
Hint: Anyone can do this.
Here’s my email to Governor Andy Beshear.
Dear Governor Beshear,
This could be the most important message you get today. I appreciate you for taking the time to read it. And first of all, let me thank you for your amazing support of patients, families, and caregivers struggling to battle the disease of addiction and its tragic effects on the lives of Kentuckians.
I was standing in that bright sun on the front row just to your right on Monday’s inspirational Recovery Month event. After attending, I am more certain than ever that KY in general, and you in particular, are truly dedicated to defeating KY’s opioid crisis — the most deadly public health emergency in our lifetime.
As I heard you speak, along with the distinguished people to your left and right, and later as I walked along that road between the Capitol and the Annex, meeting the numerous groups representing KY’s amazing response to the crisis, I really felt that united we were standing against this disease, and that we are making some progress.
And as a physician who follows scientific evidence, I’m happy I get to inform you that there is still something you can do. There’s something standing between you and your goal, but it’s fixable.
That’s good news, Governor!
I’m referring to KY’s buprenorphine regulation 201 KAR 9:270. It’s outdated and is harming the people it was intended to help. It gets in the way of KY physicians’ willingness and ability to prescribe this lifesaving medication. Something needs to be done about it. It needs to go.
I’m not a politician, not a lawyer, not a regulator. I’m a doctor. I speak for my patients, my colleagues, and the thousands of Kentuckians who could be saved by universal access to buprenorphine.
But you don’t have to take my word for it. I am certain you know of NIDA Director, Dr. Nora Volkow. I’m equally certain you trust her. Well, she has recently stated that the overdose rate in our country could be cut in half if everyone who needs buprenorphine could find access to it. Dr. Volkow has the research data to back up that claim. And, by the way, I’m meeting her at UofL tomorrow at the Louisville!Research event. Yes, I’m having a really good week!
Governor Beshear, I know in your heart and in your mind you want to do everything you can to save lives. I know it is personal to you. And I promise, if you can find some way to get rid of this outdated, unnecessary, and harmful regulation, my colleagues at KYSAM and ASAM and I will do everything we can to make certain your action in this matter will result in tremendous success — and by “success” I mean, thousands of lives saved.
Just ask yourself, is there anything else you can think of that is (a) so supported by science, (b) so supported by experts, and (c) so simple to do? You and your administration have already done so much. And you’ve had some success for sure. That’s commendable and something to celebrate. And how great would it be to stand up to the podium on the south lawn next year and be able to say that KY’s overdose deaths have been cut by 50% !
This is not just hopeful, this is do-able! Trust the science.
Governor Beshear, you work so hard, you put your heart and soul into this cause every day. You deserve to get a better return on your investment. KY needs to get a better return on your investment. And we can!
Please find some way to suspend or get rid of this buprenorphine regulation, and you will get a return on investment quantified by lives saved. I’ve already requested to meet with you along with my colleague and KYSAM President, Dr. Colleen Ryan. I hope we can make that happen soon. We’ll help you. I promise.
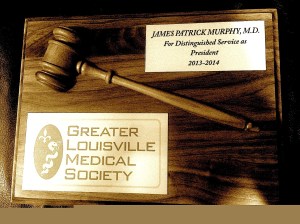
With gratitude, admiration, and respect for all you do,
James Patrick Murphy, MD, DFASAM
Director, Kentucky Harm Reduction Coalition
Region X Director, American Society of Addiction Medicine
Immediate Past President, Kentucky Society of Addiction Medicine
Assistant Clinical Professor, University of Louisville School of Medicine
Representing ASAM on the AMA Substance Use and Pain Care Task Force












 https://jamespmurphymd.com/2014/03/18/is-there-method-to-this-march-madness
https://jamespmurphymd.com/2014/03/18/is-there-method-to-this-march-madness