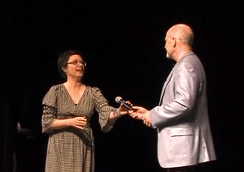
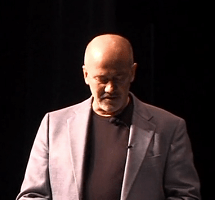
On July 28, 2013, the University of Louisville welcomed the Class of 2017 medical students. As an annual contribution to each new generation of emerging physicians, the Greater Louisville Medical Society purchases the students’ first white coat. As President, it was my honor to congratulate the students on behalf of the Greater Louisville Medical Society. Here are my remarks from the podium.
“I’m looking for someone to share in an adventure.”
Fans of the author J.R.R. Tolkein, will recognize this as the challenge Gandalf the wizard made to the hobbit, Bilbo Baggins. This is, among other things, an adventure.
I am honored to be here on behalf your medical society – The Greater Louisville Medical Society – to congratulate you on this milestone. At close to 4000 members, we are one of the largest in country. Our mission is to: promote medicine as art and science, advocate for the wellness of our community, and protect the patient – physician relationship.
Today is a big day for you and for us. Today is a milestone along the road that will lead to a your joining our ranks. Today you are not only putting on your white coats, but you are also becoming members of the Greater Louisville Medical Society. To help you stay connected you will have access to our mobile app, where you can get alerts, educational materials, and access information about your new GLMS colleagues. As sponsors of the White Coat Ceremony, your medical society colleagues are honored to provide: your first white coat, provide, your medical society pin, membership in the Greater Louisville Medical Society, professional photographic portrait of you in your new white coat. We are your colleagues, here to support you, and we welcome you.
The Greater Louisville Medical Society has strong ties to the University of Louisville. Most of our members either graduated from the University or did post-graduate training there. I am proud to call myself a graduate of the University of Louisville Medical School Class of 1985.
Back when I was in your shoes, we did not have a white coat ceremony. Back then they wouldn’t let us wear a white coat until third year, much less actually touch a living patient. I wish we could have had a ceremony like this. That is why I invited my own family to come today. This is a special day for you and for your family and friends who have supported you. To these special people in your life, I also offer my congratulations and my gratitude.
Gratitude, yes, because you have chosen a path that is not easy and does not compensate you materially for the years spent, the sacrifices, the risks – financial, physical, emotional. But it is indeed an adventure.
As I look out upon you I see a discovery. I see a cure. I see lives saved from disaster. I see longer, better, meaningful lives. I see a suicide prevented. I see a critically ill baby saved. I see an aneurysm removed. I see a heart murmur discovered. I see a cancer detected because you followed up on the red blood cells you saw in the urinalysis report.
I also see heartache, depression, fractured lives, and failures. It is all part of the path you have chosen to follow. You may not know all the reasons why you are sitting here today. I don’t think I knew. But every day, from this day forward you will be finding answers.
The white coat itself is significant. I remember the day I finally got mine. We walked around the medical complex and even went to eat lunch in one of the hospital cafeterias. In my 3rd year of medical school Dean Ganzel was my attending on rotation through Otolaryngology. On the last day she, so graciously, took her four medical students to lunch. We ate lunch at the Kentucky Center for the Arts in our white coats. The coat meant something. It said something to the world.
I have worn many white coats since them – short, long, in between – but whenever I put on the coat it still has meaning. It speaks. So I wondered what the message would be if instead of me, my white coat could says a few words. Well, my white coat and I discussed it and now, on behalf of my white coat, I offer this:
a white coat
I symbolize
the goals you hope
to realize
a white coat
my color’s pure
to show your values
will endure
a white coat
I will glisten
if you can try
to mostly listen
a white coat
in my presence
comfort, care and
convalescence
a white coat
wear this fashion
only if
you share my passion
a white coat
for my profession
put patients first
make no concession
a white coat
answer alarm
with answers that
first do no harm
a white coat
hear the calling
wear me when
you lift the falling
a white coat
my fabric must
be nothing but
a weave of trust
a white coat
ability
tailored with
humility
a white coat
a solemn oath
a way of life
or maybe both
a white coat
I’m going to
forever be
a part of you
Dean Ganzel, colleagues, friends and families, Mom, I thank you for this day. And to the class of 2017, I congratulate you and welcome you. For those who hear this calling there is no greater professional honor than to wear that white coat and hear the words, “That’s my doctor.”
Looking out at you, it is clear that I have found someone to share in an adventure.
… and the white look is very becoming, I must say.
*
This year’s White Coat Ceremony was held on July 27, 2014 and is the subject of current GLMS President, Dr. Bruce Scott’s September eVoice.
*